Dr. Kaiser RajaKings College Hospital Dubai, UAE.
Consultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced Endoscopy
Do you suffer fromFatty Liver and Liver Fibrosis?
Fatty liver disease (FLD) refers to a condition where there is an excessive buildup of fat in the liver cells.
Do you suffer from Gallstone?
Gallstones are small, hard deposits that form in the gallbladder, a small organ located just beneath...

Dr. Kaiser Raja
Consultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced Endoscopy
Dr. Kaiser is one of the very few dedicated hepatologists in Dubai and United Arab Emirates. He is highly experienced in management of all forms of complex liver diseases such as liver cirrhosis, portal hypertension, chronic hepatitis B and C, autoimmune hepatitis, acute liver failure, alcoholic liver disease, hemochromatosis and fatty liver disease.
He has a vast experience in the management of liver cancer and can help you coordinate multidisciplinary treatment of liver cancer with surgeons, interventional radiologists and oncologists. Dr. Kaiser also specialises in the management of children with liver diseases such as autoimmune hepatitis, Wilson disease, metabolic liver diseases and cholestatic liver disorders.
Specialized in :
Patient Care and Health Information
You may consult us for any of the conditions listed below. For reliable information, we've included trusted links.
Liver cirrhosis is a progressive liver disease in which healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly.
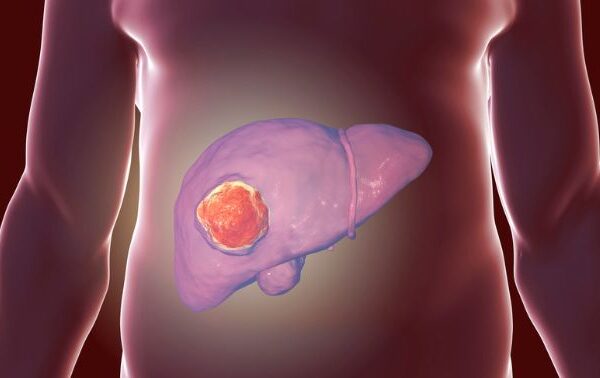
Liver cancer, also known as hepatocellular carcinoma (HCC), is a type of cancer that begins in the liver, the large organ located on the right side of the abdomen.
A liver transplant is a surgical procedure where a diseased or failing liver is replaced with a healthy liver from a donor.
Fatty liver disease (FLD) refers to a condition where there is an excessive buildup of fat in the liver cells. While it’s normal for the liver to contain some fat,
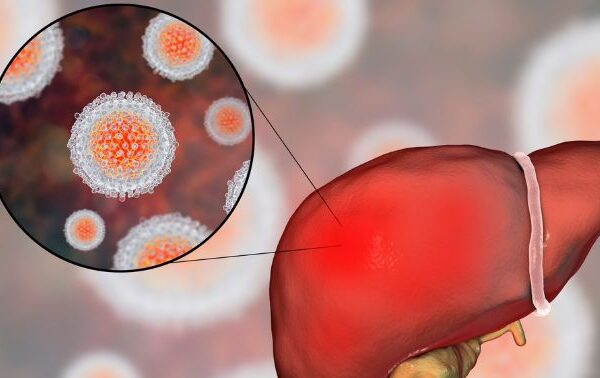
Hepatitis B and Hepatitis C are viral infections that affect the liver, causing inflammation and potential liver damage.
Autoimmune Hepatitis (AIH) is a chronic inflammatory liver disease that occurs when the body’s immune system attacks its own liver cells, mistaking…
Alcoholic Liver Disease (ALD) refers to liver damage caused by excessive alcohol consumption over time. It is a progressive condition that develops..
Gallstones are small, hard deposits that form in the gallbladder, a small organ located just beneath your liver. The gallbladder stores bile…
Pancreatitis is the inflammation of the pancreas, a vital organ located behind your stomach. The pancreas plays a key role in digestion…
Testimonials / Google Reviews
Please read how patients felt about our care and professional opinion.










Latest News & Bogs
Latest News & Recent Story From Our Blog
View this post on Instagram A post shared by Kaiser Raja (@kaiser.raja.md) Autoimmune hepatitis is a rare but serious liver condition where the body’s immune system attacks the liver, causing acute inflammation. ⚠️ Common symptoms:Yellowing of eyes (jaundice), dark urine, itching, fatigue, loss of appetite, and upper abdominal discomfort. It often affects young people, especially […]
Read MoreView this post on Instagram A post shared by Kaiser Raja (@kaiser.raja.md)
Read More3 months post liver transplant and already back on the bike!Philipa’s strength, determination, and spirit are unmatched. Morning rides never looked this powerful. Here’s to health, hope, and unstoppable energy!
Read More✨ Grateful & Honored ✨ I’m deeply humbled to share that I have been recognized by the Forttuna Global 100 Legacy Makers 2025. What makes this moment even more surreal is seeing my name and photo showcased on a billboard in Times Square, New York. This milestone is not just mine — it reflects the […]
Read MoreKings Liver Support Group Update Today, under the guidance of Dr. Kaiser, we had an insightful one-to-one Q&A session with patients and their families, focusing on life post-transplant and community support. We also had the opportunity to conduct a practical workshop with patients, led by Dr. Kaiser, which added great value to the session. A […]
Read MoreKings Liver Support Group Dubai Dr. Kaiser RajaConsultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced EndoscopyKings College Hospital London Call: +971 4 247 7777 / Whatsapp +971557181328Email: kaiser.raja@kch.aewww.drkaiser.ae
Read MoreCelebrating the incredible journey of our post-transplant warrior, Mr. Jasbir Singh, on his special day! 🎉Wishing you endless health, happiness, and success ahead. Here’s to many more milestones and birthdays!Happy Birthday, Jasbir! 🎂✨With Dr. Kaiser & Team*
Read MoreIn this inspiring journey, Mr. Punjabi a 63-year-old patient underwent a life-saving liver transplant at King’s College Hospital Dubai. From the initial diagnosis of liver cirrhosis, early-stage cancer, and additional health challenges like advanced heart disease, Mr. Punjabi’s story is a testament to the expert medical care at King’s Liver Transplant Centre of Excellence, and […]
Read MoreCertificate of Appreciation: Health Screening and Awareness Camp held on 26th July 2025 at AG Marbles, Al Quoz. Dr. Kaiser RajaConsultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced EndoscopyKings College Hospital Dubai Call: +971 4 247 7777Whatsapp +971557181328Email: kaiser.raja@kch.aewww.drkaiser.ae
Read MoreKing’s College Hospital London in Dubai has successfully completed 14 liver transplants within the first year of launching Dubai’s first adult liver transplant centre. This milestone was recently celebrated during an event at the hospital, attended by senior hospital officials, as well as medical and nursing staff.
Read MoreThe Silent Epidemic: What You Don’t Know Can Hurt You Millions of people around the world are living with hepatitis and don’t even know it. Hepatitis B and C — two of the most common forms — often show no symptoms until the disease is advanced. Every year, over 3 million new cases are reported, […]
Read MoreWe are proud to introduce Dubai’s first dedicated Paediatric and Adult Liver Transplant Centre, marking a pivotal chapter in a legacy of over 40 years of pioneering liver care!
Read MoreThe most common cause of chronic liver disease. Usually causes no symptoms. Can progress to liver cirrhosis. Fatty liver is an extremely common condition usually detected incidentally on an ultrasound scan. It develops in individuals who are overweight, and in those with diabetics. Even people with mild obesity and especially abdominal obesity are prone to […]
Read More🩺✨ Join Us at the 5th Annual Dubai International Gastroenterology Congress!📅 Date: 24–25 May 2025📍 Location: Dubai, UAE 🎙️ Featured Speaker:Dr. Kaiser RajaConsultant in Gastroenterology & Liver DiseaseKing’s College Hospital, UAE 🧠 Topic: Management of Decompensated Cirrhosis: What’s New
Read MoreAlcoholic liver disease is a result of overconsuming alcohol that damages the liver, leading to accumulation of fat in the liver, inflammation, and scarring. It can lead to cirrhosis and can be fatal. Most individuals who consume excessive alcohol may not be aware of ongoing liver damage. We recommend a comprehensive evaluation of liver disease, including […]
Read MoreA Morning of Strength, Support and Steps! 🚶🚶♀️🚶♂️ What a fantastic start to the day for our Liver Transplant Support Group! Together, they walked 4 km and took 6,750 steps filled with positivity and resilience along Dubai Marina. We look forward to this becoming a weekly tradition for health, connection, and encouragement! Dr. Kaiser RajaConsultant […]
Read More[vc_row css=”.vc_custom_1703148958767{padding-right: 0px !important;padding-left: 0px !important;background-color: #edf2fb !important;}”][vc_column][vc_empty_space height=”22px”][/vc_column][/vc_row][vc_row css=”.vc_custom_1703148966780{padding-right: 0px !important;padding-left: 0px !important;background-color: #edf2fb !important;}”][vc_column][vc_single_image image=”7455″ img_size=”full” alignment=”center”][vc_empty_space height=”22px”][vc_custom_heading text=”Our First Liver Transplant at King’s College Hospital London in Dubai, United Arab Emirates” font_container=”tag:h5|text_align:left|color:%230a2544″ use_theme_fonts=”yes”][vc_empty_space height=”10px”][vc_column_text]Our Liver Team at King’s College Hospital performed the first liver transplantation in the Emirate of Dubai. The fortunate […]
Read MoreGuests of Honour for the Forttuna Global Excellence Awards 2024! Dr. Kaiser Raja – Director of the Hepatology And Liver Transplantation Program at King’s College Hospital London, UAE
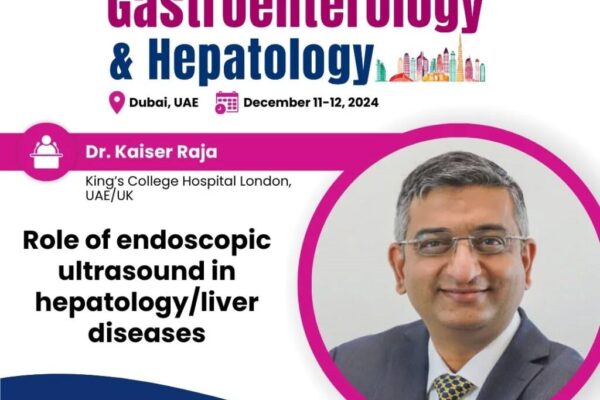
Read MoreJoin us as we delve into the revolutionary Role of Endoscopic Ultrasound in Hepatology and Liver Diseases with the distinguished Dr. Kaiser Raja from King’s College Hospital London, UAE! 🏥✨ 🔍 Discover how cutting-edge endoscopic ultrasound is transforming the diagnosis and management of complex liver conditions.💡 Gain insights into the latest advancements in liver disease […]
Read MoreOctober is Liver Cancer Awareness Month, which is a chance to raise vital awareness to improve early detection of the disease as well as showing support for people affected by liver cancer and remember loved ones.
Read MoreDr. Kaiser Raja, Consultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced EndoscopyKings College Hospital London
Read MoreThis is a form of inflammatory disease affecting the colon. It leads to loose stools often mixed with blood. A colonoscopy is needed for diagnosis. There are good long term treatment options and the disease can be controlled very well. Newer biological drugs have completely changed the treatment landscape. You can contact us in case […]
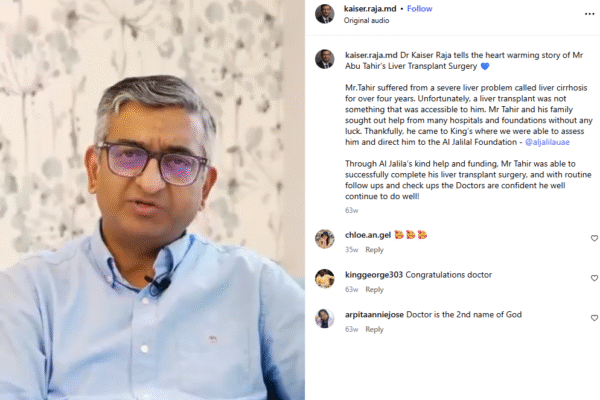
Read MoreMr.Tahir suffered from a severe liver problem called liver cirrhosis for over four years. Unfortunately, a liver transplant was not something that was accessible to him. Mr Tahir and his family sought out help from many hospitals and foundations without any luck. Thankfully, he came to King’s where we were able to assess him and […]
Read MoreMost important aspects of post-liver transplant care involves regular monitoring of liver functions and management of immunosuppression drugs. After the initial 2-3 years, most transplant patients actually need a very small dose of medications to prevent rejection. In the long term, patients with liver transplant are prone to develop diabetes, hypertension, cardiac disease and most […]
Read MoreWatch as Dr Kaiser Raja, talks about all things Liver and the first successful Liver Transplant in Dubai right here at King’s College Hospital Dubai. If you have any questions please fell free to contact with us.
Read MoreView this post on Instagram A post shared by Kaiser Raja (@kaiser.raja.md) We are proud to announce that we have completed 6 successful liver transplantations. A huge thank you to our excellent liver transplant centre team and to the donors and their families who’s selfless decisions have changed lives!
Read MoreLiver Transplant Support Group Join our upcoming Liver Transplant Support Group meeting a supportive space for recipients, caregivers, and family to connect and share experiences. Let’s Join UsJuly 25th, 2024 05.00 PM – 07.00 PMKings College Hospital LondonDubai, Dubai Hills. Location:https://maps.app.goo.gl/cB44iA8ns4J1oroe6
Read MoreThe Bravery Blueprint: Dr. Kaiser Raja | FFTB 02 – Dr. Kaiser Raja x Raul Handa | The FFTB Show Dr. Kaiser RajaConsultant in Liver Diseases, Transplant Hepatology, Gastroenterology and Advanced EndoscopyKings College Hospital London Call: +971 4 247 7777 / Whatsapp +971557181328 Email: kaiser.raja@kch.ae www.drkaiser.ae Location:https://maps.app.goo.gl/cB44iA8ns4J1oroe6
Read MoreMay is Hepatitis Awareness Month in the U.S. Globally, 354 million people live with viral hepatitis in the world today Every year, more than a million lives are lost to hepatitis. We’re not waiting for change – we’re fighting to make it happen. more than 1.2 Million lives are lost each year to hepatitis B and […]
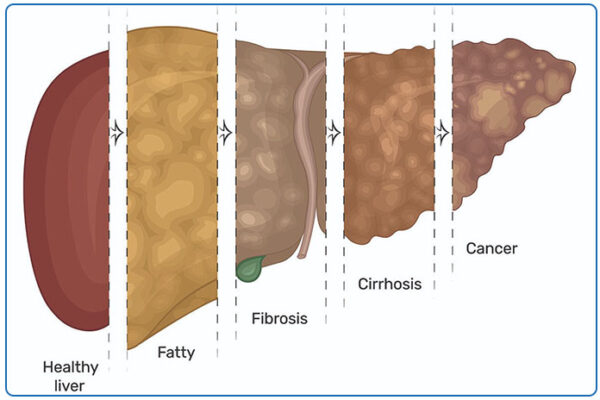
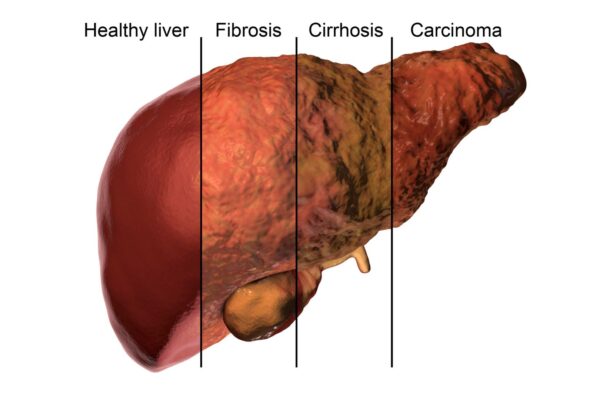
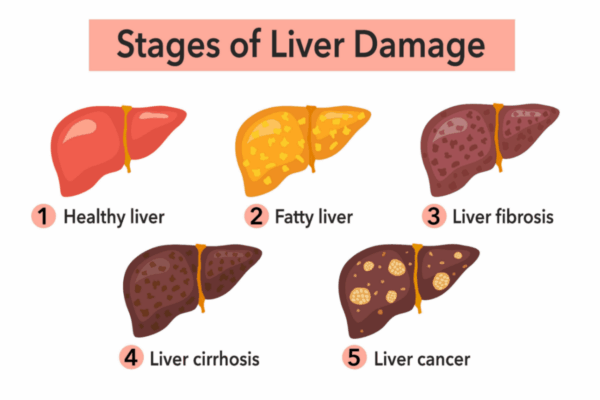
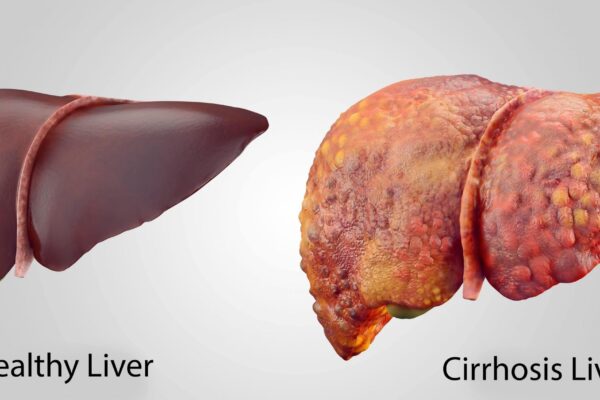
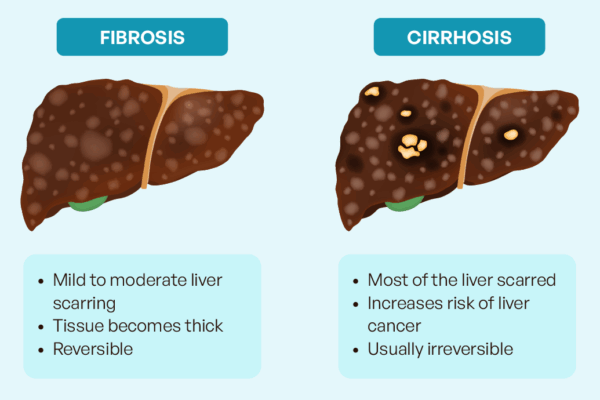
Read MoreExtreme liver fibrosis is known as liver cirrhosis. In this condition, the liver which is otherwise a soft organ becomes quite hard and starts functioning poorly. Patients can go on to develop liver failure in which there is development of jaundice (yellow eyes), generalized weakness, loss of muscle mass, accumulation of fluid in the belly […]
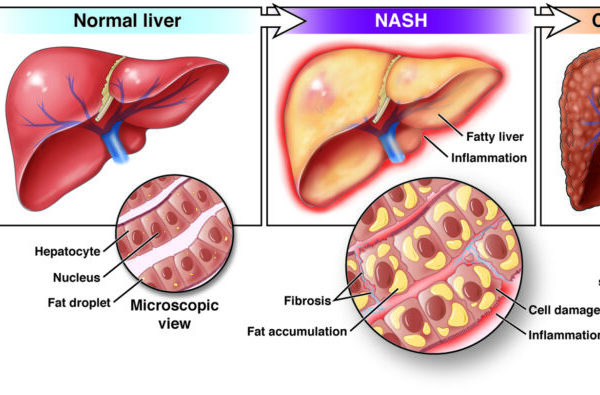
Read MoreThis is the most important differentiation to be made when a patient seeks medical consultation for fatty liver. Simple fatty liver usually does not progress to advanced liver disease while NASH may progress over several years to more advanced forms of liver disease such as liver fibrosis and cirrhosis. Advanced NASH is also a risk […]
Read MoreFatty liver usually develops in individuals who are overweight, and in those with diabetics. Even people with mild obesity and especially abdominal obesity are prone to develop fatty liver. Fatty liver is especially common in those with a condition called metabolic syndrome. Patient with metabolic syndrome usually have a combination of one of more of […]
Read MoreSimple fatty liver without liver inflammation (also known as nonalcoholic fatty liver or NAFL). This is generally a benign condition that usually does not progress to advanced forms of liver disease. Fatty liver with liver inflammation (also known as non-alcoholic steato-hepatitis or NASH). In this condition, the excess fat in the liver causes inflammation of […]
Read MoreFatty liver disease is a medical condition in which there is accumulation of excess fat in the liver. Fatty liver has been well known to be associated with excess alcohol consumption. But Fatty Liver is also extremely common in individuals who do not drink alcohol or drink little alcohol. This form of fatty liver is […]
Read MoreWorld Liver Day is celebrated globally on April 19. The day focuses on increasing awareness of liver-related problems and diseases. The liver is one of the vital organs, responsible for immunity, digestion, and metabolism. Any liver disease or sickness affects not only the digestive system, but also the kidneys, lungs, heart, and brain. Excess fat […]
Read MoreA colonoscopy is an examination of the inside of the large intestine, which includes the entire colon, rectum and anus. It is a type of endoscopy, in which a flexible tube with a camera at one end (colonoscope) is inserted into your body. The colonoscope passes through your anus and rectum into your colon. This is […]
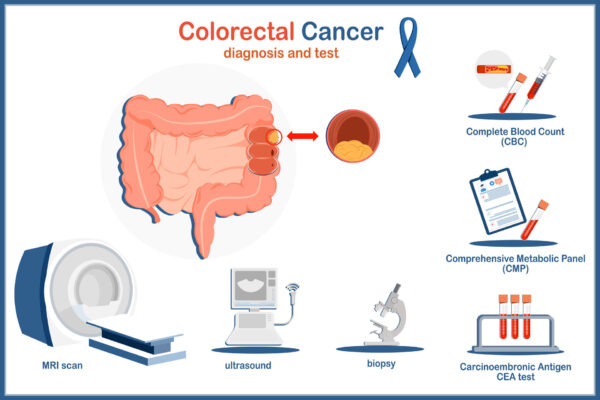
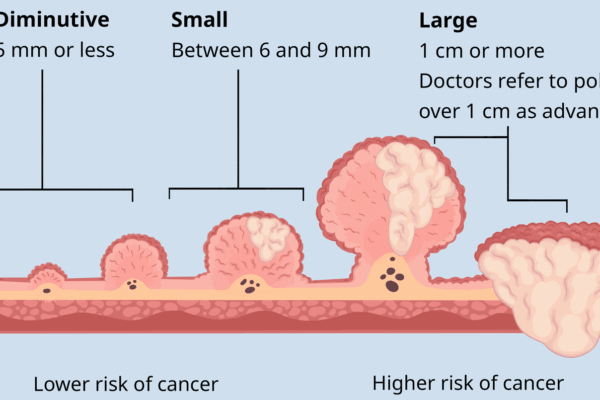
Read MoreScreening involves direct visualization of the inner lining of the colon to detect polyps. This can be done either by colonoscopy or sigmoidoscopy. Non-invasive techniques such as virtual colonoscopy using a CT scan can also visualize the colon lining. Other colon cancer screening tests involve stool analysis for presence of occult blood which may indirectly […]
Read MoreNinety percent of all colon cancers start as polyps. Therefore, the best way to prevent colon cancer is to look for precancerous polyps inside the colon and remove them before they progress to cancer. Colorectal cancer screening tests are designed to find precancerous polyps. Screening also detects cancers at an earlier stage when complete cure […]
Read MoreRole of Endoscopic Ultrasound in Hepatology/Liver Diseases International Conference on Advances in Gastroenterology and HepatologyGastroenterology 2024 Multidisciplinary Approaches to Digestive Health: Collaborating for Better Outcomes April 19-20, 2024, Dubai, UAE
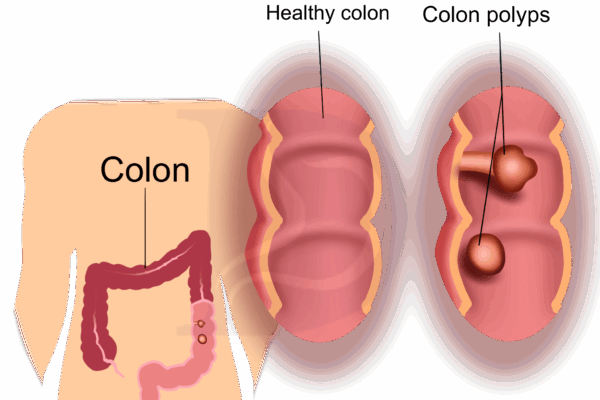
Read More[vc_row][vc_column][vc_custom_heading text=”What are colon polyps and why should you look for them?” font_container=”tag:h5|text_align:left|color:%231e73be” google_fonts=”font_family:Prata%3Aregular|font_style:400%20regular%3A400%3Anormal”][vc_empty_space][vc_empty_space height=”10px”][/vc_column][/vc_row][vc_row][vc_column width=”1/2″][vc_custom_heading text=”What are colon polyps?” font_container=”tag:h5|text_align:left” use_theme_fonts=”yes”][vc_column_text]A colon polyp is a growth on the inner lining of the colon (large intestine) or rectum. Polyps in the colon arise from uncontrolled multiplication of cells leading to growth of tissue. This can […]
Read MoreMost colon polyps and early colorectal cancer do not have any symptoms, which is why screening is recommended. However, when symptoms do occur, they may include:
Read MoreColorectal cancer is the third most common cancer worldwide. Almost 2 million cases are diagnosed every year. It is the second most common cause of death due to cancer, leading to almost 1 million deaths per year. It is estimated that the incidence of colon cancer will increase by almost 50% in the next 20 […]
Read MorePolyps are found in about 30% of the adult population over the age of 45. Men and women of all ethnicities are at risk of developing colon polyps.Many factors including diet, lifestyle, older age, and genetics increases the risk for polyps. Important factors predisposing to colorectal polyps and cancer include:
Read MoreEssentially there are two types of polyps. Hyperplastic polyps which are not pre-cancerous and adenoma type of polyps which are pre-cancerous. The type of the polyp can be determined only after its removal.
Read MoreA colon polyp is a growth on the inner lining of the colon (large intestine) or rectum. Polyps in the colon arise from uncontrolled multiplication of cells leading to growth of tissue. This can occur due to mutation in the genes of the cells. A polyp can vary in size from few millimeters to several […]
Read MoreThe three most common diseases that cause chronic liver disease, liver fibrosis and cirrhosis are alcoholic liver disease, chronic viral hepatitis (hepatitis B and C), and non-alcoholic fatty liver disease that is usually associated with diabetes and obesity. Other diseases such as autoimmune hepatitis, and excess of iron in the body known as hemochromatosis can […]
Read MoreLiver fibrosis does not cause any symptoms and routine blood tests and ultrasound scan cannot detect liver fibrosis. It is important to detect liver fibrosis at an early stage so that its progression can be prevented. If untreated, liver fibrosis may progress to cirrhosis of the liver, liver failure, and liver cancer. If you have […]
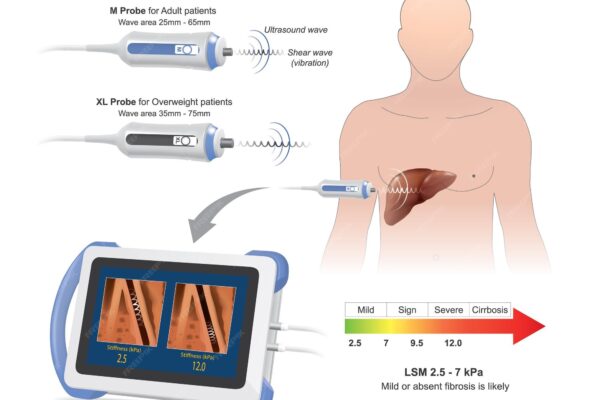
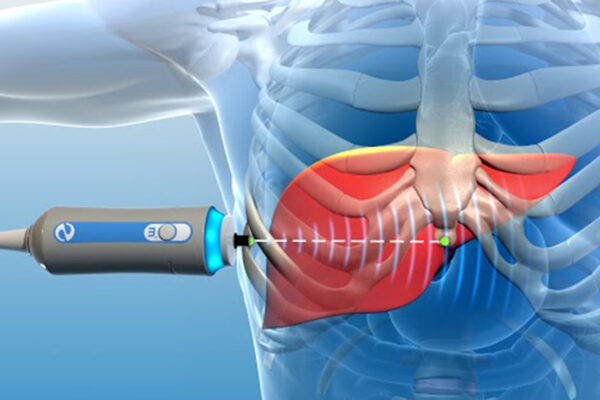
Read MoreFibroscan uses ultrasound waves using a technique called transient elastography. Liver stiffness is evaluated by measuring the speed of a vibration wave as it travels through the liver. The speed of the vibration wave is slower in a soft (normal) liver and faster in a firm or hard (fibrotic) liver. Liver stiffness is eventually expressed […]
Read MoreMany chronic liver diseases such as fatty liver, hepatitis B, hepatitis C, or excessive alcohol use can cause persistent inflammation of the liver and lead to progressive liver damage. Over a period or time, healthy liver tissue is replaced by scars. Scarring of the liver is known as liver fibrosis. Liver fibrosis results in diminished […]
Read MoreMost patients with chronic acid reflux are able to control their symptoms only by taking a daily acidity reducing pill such as Omeprazole or Nexium. There ae some who are not completely relieved even after use of these pills. If you have troublesome acid reflux, you merit a proper evaluation with an endoscopy to assess […]
Read MoreIt is recommended not to eat or drink anything for three hours before the Fibroscan. If needed, you can have small sips of water or clear fluid. You will be asked to lie flat on your back on an examination couch and to place your right arm behind your head. The examiner will feel the […]
Read MoreThe complex, four-hour-long surgery involved the complete removal of the diseased liver and the implantation of a healthy one The first liver transplant in Dubai recently took place at Kings College Hospital London- Dubai. The patient, a 38-year-old woman, suffered from a rare condition known as autoimmune hepatitis, which causes the body’s immune system to […]
Read MoreA Fibroscan is a type of scan that measures the ‘stiffness’ of your liver, which in turn reflects the degree of scarring (fibrosis) in your liver. It is a simple, painless test which gives immediate results. It does not have any potential complications or risks and is non-invasive, which means that it does not break […]
Read MoreWishing you and your family A Happy New Year filled with hope, health, and happiness.
Read MoreThe UAE National Day is celebrated yearly on 2 December to commemorate the formation of the United Arab Emirates.
Read MoreClinics in Liver DiseasesAutoimmune Hepatitis and Cholestasis: Current Knowledge and Clinical PracticeCase Presentations and Discussion Speaker Dr. Kaiser RajaConsultant in Gastroenterology and HepatologyKCH Liver Care and Transplant ProgramKing’s College Hospital London, Dubai Date: THURSDAY 30th November 2023Time: 08:30 PM – 10:00 PM (Dubai Time)Venue: JW Marriott Marquis Hotel Dubai 04 519 9999 / 971557181328Email: kaiser.raja@kch.ae
Read MoreDid you know that Diabetes is one of the major risk factor fatty liver and liver fibrosis. If you are a diabetic, make sure you have checked for liver disease. A simple FIB-4 test and Fibroscan are easy ways to check for liver disease. If you have any questions please fell free to contact with […]
Read MoreMay millions of lamps illuminate your life with endless prosperity, health, and wealth forever. Wishes you and your family a Very Happy Diwali
Read More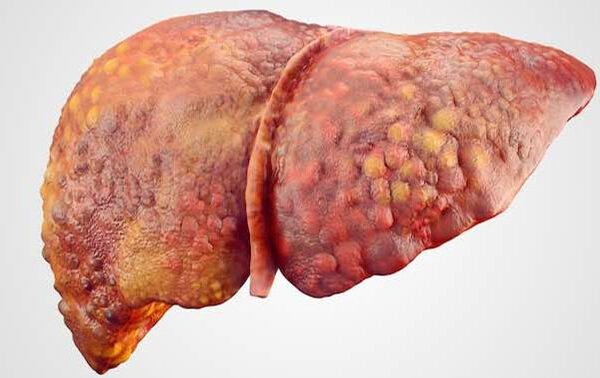





























 Get Clinic or Online Consultation
Get Clinic or Online Consultation